Author: Shabnam Narval
Affiliation: National Institute of Immunology, New Delhi, India.
Date: 4th January 2025
The COVID-19 pandemic has reshaped the landscape of global health and spotlight has been shifted towards respiratory health. In the relentless battle against COVID-19, pneumonia has emerged as a formidable adversary, often complicating the condition of patients and contributing to the severity of the disease.
Pneumonia, characterized by inflammation of the air sacs in the lungs, remains a leading cause of morbidity and mortality across the globe, particularly among vulnerable populations such as children under five and the elderly (1).
According to the World Health Organization (WHO), pneumonia is responsible for an estimated 2.5 million deaths annually, with the majority occurring in low and middle-income countries where access to healthcare and preventive measures may be limited (2). There are many causative agent for pneumonia like bacteria, fungi and viruses.
Bacterial infection tends to be more severe and common reason for death of the vulnerable group which are children and elderly. The most common and aggressive bacterial culprit for community acquired pneumonia is Streptococcus pneumoniae. This bacteria lurks in nasal cavity of healthy individuals seeking for an opportunity that are yet to be fully understood. The invasion of the lungs by these bacteria leads to pneumonia, and if left untreated, the infection can worsen, reaching the bloodstream and causing septicemia (3).
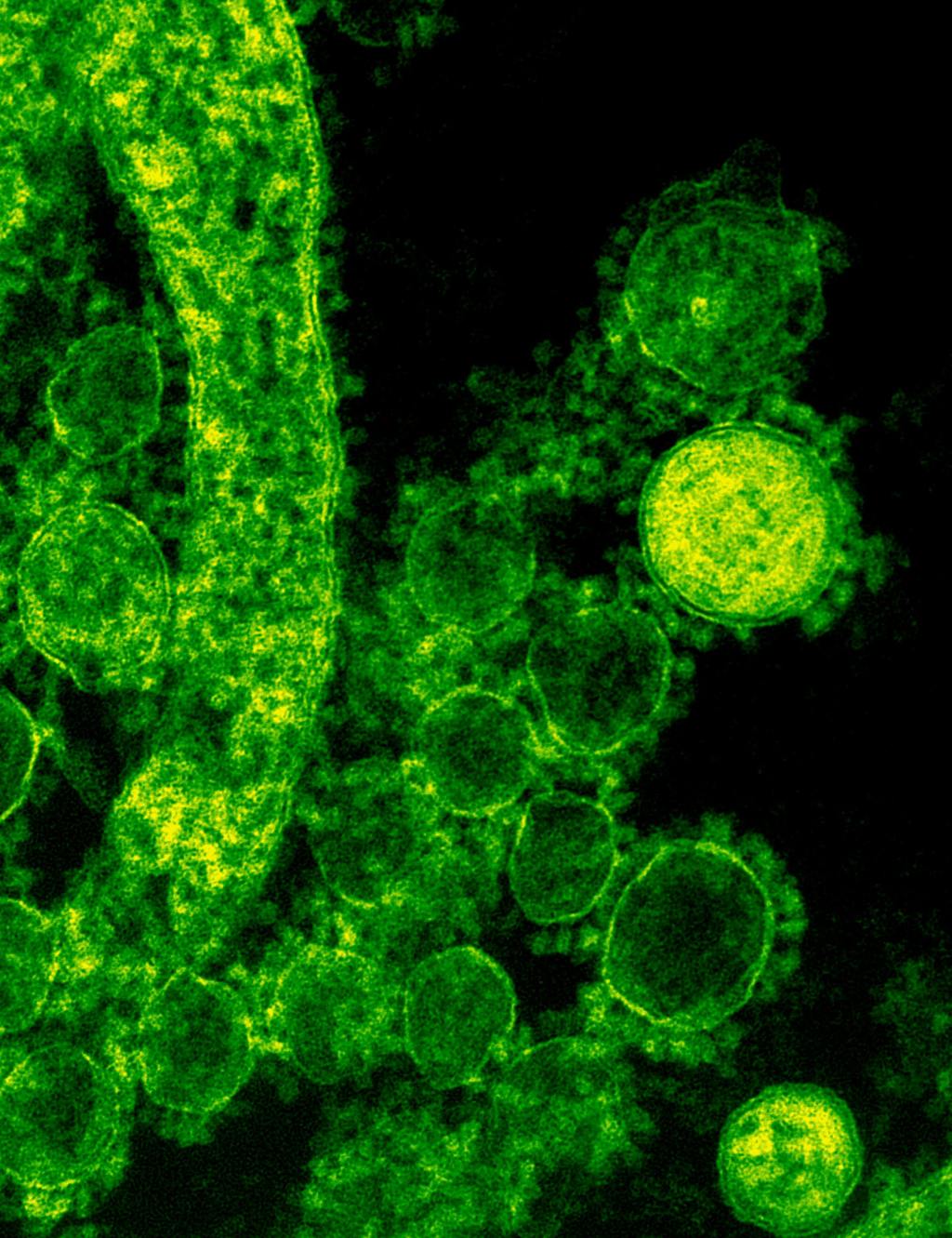
The main culprit is the bacteria’s sugar coating (polysaccharide capsule), which helps them evade the immune system by preventing detection and phagocytosis. This shiny capsule facilitates colonization of the nasopharynx and inhibits various immune responses, such as phagocytosis and the complement system, ensuring a successful infection (4,5). As a result, the bacteria’s virulence and resistance to host defenses increase, making them more capable of causing severe pneumonia, particularly in vulnerable individuals.
At present, depending on the composition of sugars present in capsules, more than 100 serotypes of the pneumococci are found. This layer usually consist of simple sugars (monosaccharide) like glucose, galactose in repetition. Diagnosing pneumonia can be challenging, as its symptoms—fever, cough, chest pain, and difficulty in breathing—often overlap with those of other respiratory conditions.
Healthcare providers typically rely on a combination of clinical evaluation, chest X-rays, and laboratory tests to confirm the diagnosis. Timely initiation of appropriate treatment is paramount, usually involving antibiotics. The serendipitous discovery of penicillin by Alexander Fleming in 1928, played an instrumental role in controlling bacterial pathogen like pneumococci. However, their indiscriminate use has led to the development of antibiotic resistant bacteria.
The emerging threat of antibiotic resistant pneumococci is predicted to reverse the medical progress that has been made over the past century and is said to be a catalyst of the next pandemic. While treatment remains crucial, prevention serves as the cornerstone to control pneumonia. Vaccination has significantly reduced the risk of pneumonia and its complications, particularly in high-risk populations.
Currently, there are two types of formulations: one consisting of the outer polysaccharide (sweet coating) layer alone, and the other conjugated with a carrier protein. As both formulations carry a polysaccharide layer specific to a serotype, they render these vaccines serotype-dependent (6).
Nowadays, serotypes not covered by vaccines are responsible for causing the disease. Researchers in this field are working tirelessly with the aim of discovering a protein candidate which can be used as a potential vaccine candidate. It will solve the problem of less serotype coverage as proteins are usually conserved across serotypes because of their specific function. With the advancement of artificial intelligence, it is hoped that scientists will be able to solve this problem in the coming years.
References
- Lim WS. Pneumonia—Overview. Encyclopedia of Respiratory Medicine 2022:185–97. https://doi.org/10.1016/B978-0-12-801238-3.11636-8.
- World Health Organization, 2025. Pneumococcal disease. Available at: https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/norms-and-standards/vaccine-standardization/pneumococcal-disease [Accessed 4 January 2025].
- Weiser, J.N., Ferreira, D.M. and Paton, J.C., 2018. Streptococcus pneumoniae: transmission, colonization and invasion. Nature Reviews Microbiology, 16(6), pp.355-367.
- Mitchell, A.M. and Mitchell, T.J., 2010. Streptococcus pneumoniae: virulence factors and variation. Clinical Microbiology and Infection, 16(5), pp.411-418.
- Paton, J.C. and Trappetti, C., 2019. Streptococcus pneumoniae capsular polysaccharide. Microbiology spectrum, 7(2), pp.10-1128.
- Kim, G.L., Seon, S.H. and Rhee, D.K., 2017. Pneumonia and Streptococcus pneumoniae vaccine. Archives of pharmacal research, 40, pp.885-893.